Artwork Fleur Wickes
It’s well documented how difficult treatment for breast cancer can be, but Síana Clifford discovered that the period after is a tricky time too – and that connecting with your own cancer crew is the best medicine.
I know I’m supposed to be in a good mood and feel so lucky it’s all over but I’m in a really bad place and struggling with the side effects. I can’t pretend that this is easy and I feel lucky anymore. These last few days have probably been the hardest.
I wrote this in my journal a few days after I finished radiotherapy treatment for breast cancer last year. I assumed I’d be feeling on top of the world when my treatment was over, celebrating that any cancerous cells inside my body had been vanquished and I was able to resume my “normal” life.
I was supposed to feel happy and grateful.
And I was grateful to be done with treatment, hugely grateful for the public health system in Aotearoa New Zealand and so very grateful that the cancer chapter was over, hopefully for good.
But, even as work deadlines ramped up again and I began to fill my calendar back up, it really didn’t feel like that cancer chapter was actually over.
Apart from having burnt, sore and broken post-radiotherapy skin, crippling fatigue (which would last for months) and the beginnings of lymphatic issues in the cancer boob (see below onlymphoedema), it also felt like all the mental and emotional aspects of the experience were only beginning to hit me, just at a time when everyone was expecting to have the normal Síana back.
Down on your luck
The “lucky” I referred to in my journal entry above was very much at odds with what I was feeling too.
Comparatively, there’s no doubt I had been very lucky with my cancer experience.
It was discovered in a very serendipitous fashion and was caught super early – if you’re going to get breast cancer, this is the one you want.
Treatment-wise, I had a lumpectomy and 15 blasts of radiotherapy, but I didn’t require chemotherapy, the more drastic body alteration that a full mastectomy entails or any ongoing medication.
I was also so lucky to be in probably one of the best places in the world to be experiencing cancer during Covid-19.
I was diagnosed two days into the first lockdown and it looked like my surgery might be delayed but then our lockdown worked so well it went ahead on schedule.
I knew that all that made me very lucky indeed, and I was sure to express that in every conversation I had about my cancer: it could be worse, I was so fortunate it was found the way it was, etc.
But I still had cancer. And cancer, even the “good” kind, is crap. Having cancer during a global pandemic, so I couldn’t get home to my family in Ireland or have any visitors in hospital, is even crapper.
And the emotional and mental aftermath of all of that crap is what I was feeling rather than the happy days and sweetness and light I had been expecting to feel – and sometimes felt that others were expecting from me.
What the hell was wrong with me that I felt so bad?

Untangling tangled emotions
It turns out that this is not an uncommon way for women to feel once they’ve finished active treatment for breast cancer.
One day I put up a post in the Aotearoa Breast Cancer Community Facebook group that I’d been lurking in about how fatigued and down I still felt weeks after radio.
The support and empathy came flooding in. I met some of those kind women who had responded for coffee and that’s when I realised that my post-cancer experience was far from abnormal.
Over that coffee, and during chats with many other women in the ‘cancer club’ since, we talked about how while you’re going through treatment you’re juggling all the appointments and the practicalities of the treatment itself.
You’re in survival mode, concentrating on getting through each of your treatment steps.
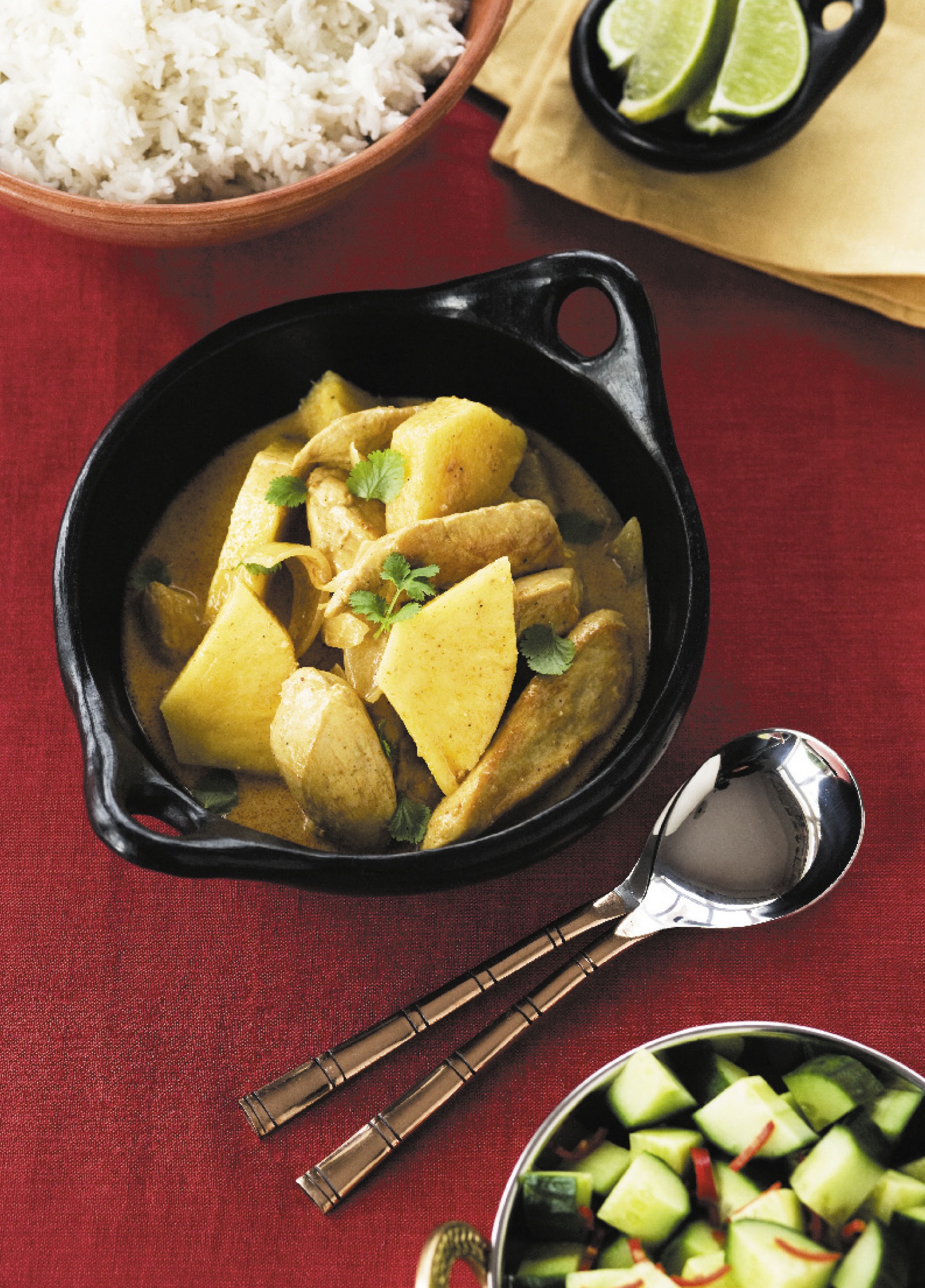
Hopefully you have a support crew, who are maybe dropping off meals, sending gift hampers or offering to drive you to treatment, clean your house or look after the kids.
Once all that stops and you actually have time for everything to sink in, and the support crew have fallen away – and that’s fair enough, no shade intended, as far as they’re concerned you’ve beaten cancer now and their job is done – that’s often when your mind and emotions catch up.
Suddenly you’re dealing with the aftermath of this huge event in your life that has led to you confronting the reality of your mortality.
There might be anger (why did this happen to me?). There’s often depression, or at least low mood. Your body has changed, which might impact how you feel about being intimate with anyone.
For others, there might have been a shift in some of their core relationships after the painful realisation that some of the people in their lives weren’t there when they needed them.
There’s a kind of grieving period involved in all of that. You’re looking at the world, your relationships, your priorities, your body and even yourself as a person differently now.
You’re grieving for the life you once lived, the body you once had and the person you used to be.
You’re wondering who you are now and what is ahead for you (and yes, whether cancer is going to feature again).
These emotions aren’t easy to process as the person going through them, let alone for those around you to understand, when they were probably expecting only positive emotions from a cancer “survivor”.
On top of that the physical side effects of cancer treatment, don’t neatly end when treatment does.
Many still have reconstructions or other aesthetic surgeries ahead of them – I know I still have one more to go. You’ll likely need physio to deal with the aftermath of surgeries and radiotherapy.
Lymphoedema is an after-effect that can appear in the months or even years after treatment. And the fatigue, oh the fatigue can linger for so long, which can make that “normal” life you’re supposed to be striving to return to feel very out of reach indeed.
The scourge of scanxiety
One of the things that took me by surprise about the end of active treatment is that you don’t get a mammogram to check they’ve got everything.
One day you are just… finished.
There’s almost a sense of anti-climax, as there’s no appointment with your oncologist where they hold up a scan and proclaim that you’re cured.
You have to just have faith that the treatment protocol did its job and all those pesky cancer cells have been cancelled.
That faith can waver of course and for a while, any twinge can send you into a scare spiral that it’s coming back.
You’re officially monitored for five years after cancer, so soon enough mammogram time rolls around again.
And that’s when the anxiety (or scanxiety) really kicks in – that fear of what might be discovered when the memory of what the last found is so fresh.
The doctors are, as always, pragmatic and your support crew is full of positivity, but in the dead of night in the weeks leading up to that scan, you’re remembering how it wasn’t all right the last time.
And so how can you presume it will be this time? It’s undeniably a logical and legitimate fear, yet you don’t want to let the side down by voicing it.
Cancer really is the gift that keeps on giving.
The good news
My mammogram was all clear, yay! It felt great to have that first annual one done and hopefully the next ones will be less anxiety-inducing (ask me again next April).
The even better news is what I know now, about a year since that tough post-treatment period began.
I know now that all of the emotions I was feeling (and sometimes still do), as unexpected and difficult as they were, are totally normal. And just knowing that does take some of the weight from them.
I also know now that it was connecting with other women who had and have breast cancer that has made all the difference to me.
That first post in the supportive corner of the internet that is the Aotearoa NZ Breast Cancer Community Facebook group (shout out to founder Belinda Tran-Lawrence for taking the initiative and time to set it up) enabled me to connect online and in real life with people who knew exactly how I was feeling.
There’s nothing like sharing experiences with people who have been there too and who totally get it, all of it. When you’re feeling alone in something there is such immeasurable power in that.
The cancer community
There’s a lot of help available to women with breast cancer, it’s just that you just don’t always know about it.
Schemes like the Pink Ribbon card offered by BCFNZ to fund physio are well known, but did you know you could also get involved in dragon-boating, an exercise class designed especially to get you moving after cancer or even paddle-boarding?
Or that you can be pampered for a morning with classes on skincare, make-up and wig-care during and after cancer?
Or that you could go on a fly-fishing retreat with a group of strangers who will become lovely new friends by the end of the weekend?
It was by connecting to other women that I found out about all of these experiences.
If you get involved with any of it – and I cannot recommend it highly enough that you pick something that appeals to you and go for it – you’ll meet and connect with more women who have and had breast cancer and before you know it, you have a whole circle of wāhine toa, the ultimate girl gang who you support and you know will support you.
And at a time that might just feel like the loneliest part of the cancer experience, that’s invaluable.

Look out for lymphoedema
Post-treatment, it’s vital to keep an eye out for any signs of lymphoedema.
Lymphoedema is a progressive, chronic condition that causes swelling. Lymph fluid is usually transported from the tissues to the bloodstream, but if the lymphatic drainage system is damaged, this can’t happen and swelling occurs.
It starts gradually but swelling can become permanent if untreated. It can also lead to infections that quickly become serious, e.g., cellulitis, because the lymphatic system can’t work properly to clear them.
During breast cancer treatment, many women have lymph nodes removed, or their lymphatic system might be damaged during surgery or radiotherapy, so it’s vital to be really vigilant about lymphedema.
Onset is gradual and it’s something to be constantly aware of.
If you detect swelling, aching, heaviness or stiffness in the arm, hand, breast or trunk on the side you had cancer, or have been getting infections on that side, these could be signs of lymphedema.
If caught early, it can be managed well and even reduced, so don’t wait to get tested. A lymphoedema therapist will teach you techniques (e.g., lymphatic massage) to manage swelling and may fit you with compression garments.
BCFNZ can help fund treatment via their Pink Ribbon card scheme.
Keep abreast of your breasts!
October is breast cancer awareness month, the time of year we’re reminded just how important it is to do a breast check every month.
The week after your period is a good time to schedule it – put it in your calendar as a recurring event so you don’t forget.
Check out the Breast Cancer Foundation (BCFNZ) website for a guide on how to get to “know your normal” so you’ll be able to quickly detect any changes. If you do find anything abnormal, get it checked as soon as you can.
Eligibility for free mammograms every two years with BreastScreen Aotearoa kicks in at age 45 and ends at 69 but BCFNZ recommends, if possible, paying for a private mammogram each year from 40-45 and for each alternate year between the BreastScreen checks.
You could also consider continuing them after the age of 69. When you’re going for a mammogram, try to schedule it between days 7-10 of your cycle, especially if you tend to suffer from cyclical breast tenderness.
Almost half of women have dense breasts – breasts that have more supportive fibroglandular tissue than fatty tissue.
This supportive tissue shows up white on a mammogram, just as cancer cells do, which can make cancer more difficult to detect.
So other options for women with dense breasts include having an ultrasound in combination with a mammogram or having a 3D mammogram (digital breast tomosynthesis).
A contrast mammogram is another option – you have an IV injection of the same kind of contrast dye agent used in CT scans before having a mammogram as normal. The contrast agent will show up cancers that might not be visible on standard mammograms.
It can also give a clearer picture of the extent of a cancer, meaning a patient is less likely to have to undergo multiple surgeries to get clear margins.
Dr Monica Saini is a big believer in contrast mammography. Her private practice, the Breast Institute New Zealand in Lower Hutt, Wellington is the only place to offer it in New Zealand.
Dr Saini has also used it for public patients and hopes that it can become more commonly used, especially because it is a quarter of the cost of an MRI – “this is an excellent tool we should be using at the DHB.
It just doesn’t take as much time and expertise – why are we not doing something so cost-effective?”
One Day at a Time – New Zealand artist Fleur Wickes is a favourite of mine and the artwork Wickes drew on day two of the first Covid lockdown, also the day of my diagnosis, was a particularly useful reminder during treatment.
The Rain Comes Down the Stars Come Up the Sun Rises in the Morning – This was another artwork by Fleur Wickes that I found inspirational during my cancer journey.
To see more work by artist Fleur Wickes visit her website.